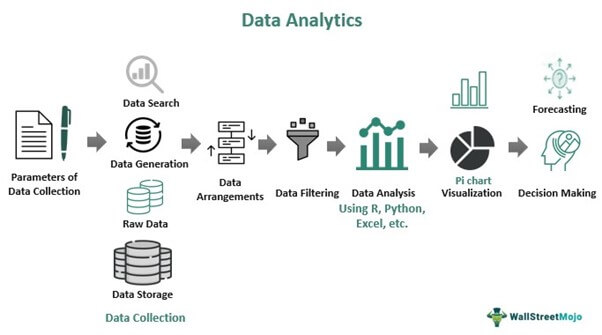
Data Preprocessing:
The algorithm starts by preprocessing the claims data, including cleaning and transforming the data into a suitable format for analysis. This step may involve removing outliers, handling missing values, and normalizing or standardizing the data